The International Federation of Psoriasis Associations (IFPA) reports that psoriasis affects 125 million people globally. While these figures highlight a significant issue, it’s crucial to remember that psoriasis is not infectious.
This chronic inflammatory skin condition manifests as red, flaky patches known as plaques. These lesions can be itchy, painful, and aesthetically displeasing, and they may form anywhere on the body, though they frequently appear on the scalp, knees, elbows, and lower back.
While the precise origins of psoriasis remain unclear, it is classified as an immune-mediated disorder. In this context, the immune system mistakenly targets healthy skin cells, leading to an accelerated growth and shedding process. This rapid proliferation results in a buildup of excess skin cells at the surface, creating the characteristic plaques associated with the condition. Fortunately, there are targeted treatments available to manage and mitigate psoriasis flare-ups.
Flare-ups can be erratic and challenging to navigate, often impacting daily activities and contributing to emotional distress. However, armed with knowledge and practical strategies, you can lessen both their frequency and intensity. One effective approach is the regular application of psoriasis cream to maintain skin hydration and minimize scaling.
Psoriasis comprises several distinct types, and understanding these variations is essential for effective treatment. Alongside the use of appropriate creams, there are additional strategies to help manage flare-ups. Here are some recommendations:
Identifying triggers that can provoke flare-ups is vital. By recognizing and steering clear of these specific stimuli, you can effectively reduce the occurrence and severity of attacks. Common triggers include stress levels, certain climatic conditions, and dry skin.
Addressing stress through relaxation techniques, physical activity, or sufficient sleep can prove beneficial. If necessary, seeking guidance from mental health professionals can provide tools to manage stress or anxiety effectively. Interestingly, warm weather may sometimes alleviate psoriasis symptoms due to elevated humidity; however, it remains essential to apply sunscreen and limit exposure to direct sunlight and excessive sweating, as these factors can also provoke flare-ups.
Triggers can differ significantly among individuals. Keeping track of what exacerbates your psoriasis and discussing these insights with your healthcare provider can enhance your management strategy. Dry skin typically exacerbates symptoms, leading to increased itching, redness, and discomfort. Keeping the skin well moisturized can help diminish inflammation and improve its overall texture.
Applying a rich, fragrance-free moisturizer immediately after bathing, while the skin is still damp, can seal in moisture. Opt for products containing ingredients like glycerin, hyaluronic acid, or urea, which aid in moisture retention within the skin.
Topical treatments such as creams and ointments featuring active compounds can assist in reducing inflammation and normalizing skin cell production. Various topical remedies are available for psoriasis, and consulting your healthcare provider is crucial to determine which products are most suitable for your specific skin condition.
Another treatment option is light therapy, where affected skin is exposed to ultraviolet (UV) light to decrease inflammation and slow down skin cell proliferation. The two forms of UV light utilized for psoriasis treatment are UVA and UVB. UVA is typically administered in a clinical environment, whereas UVB is something that can be applied at home with specialized equipment.
Prior to initiating light therapy, it’s advisable to consult a healthcare professional to establish the most beneficial treatment pathway for you. It’s important to note that light therapy may come with side effects, including sensations of burning, itching, or skin redness, and it might not be suitable for everyone.
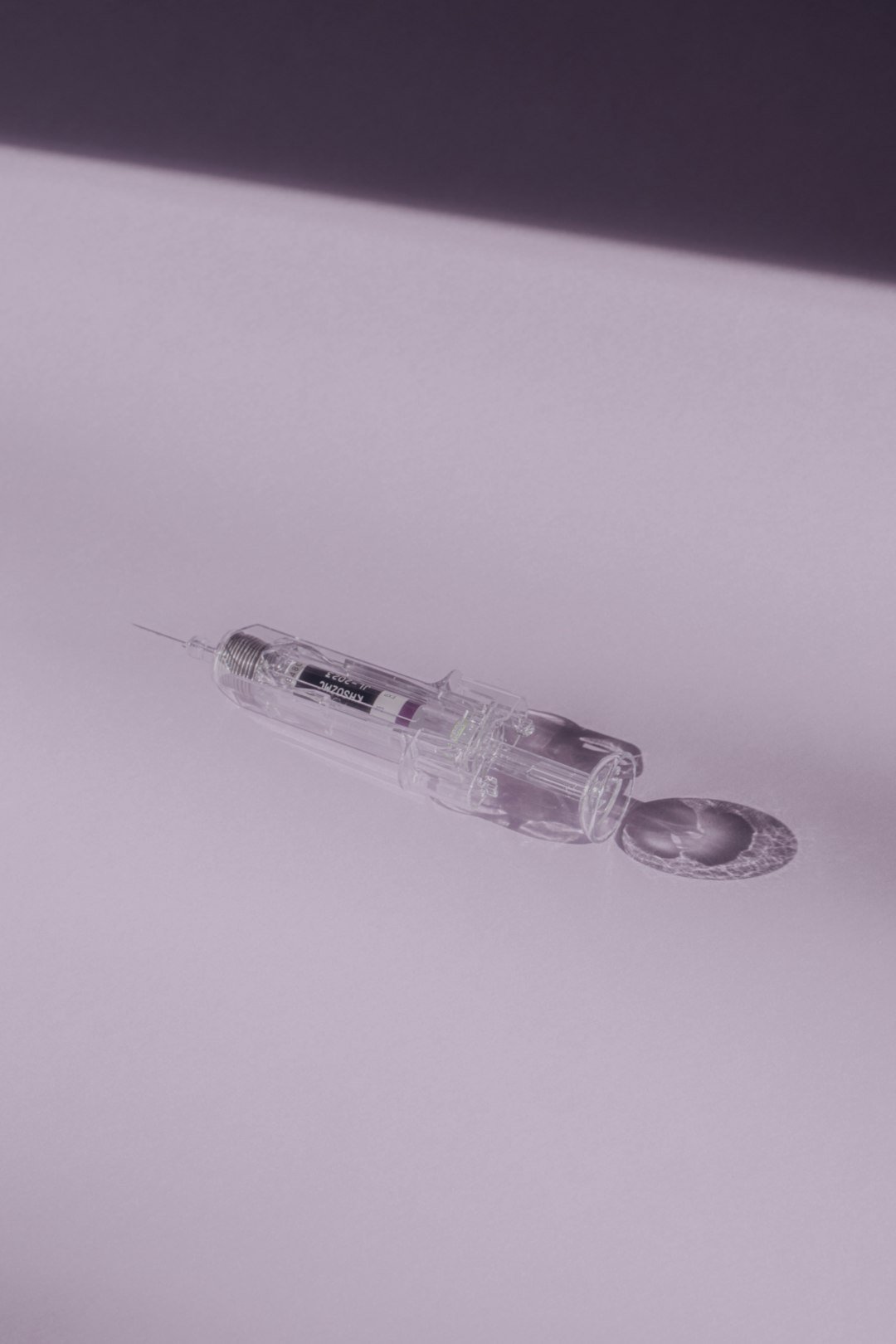
Injectable medications present another avenue for the management of psoriasis flare-ups. These treatments work by suppressing the immune response and decelerating skin cell growth. They are usually reserved for cases where other therapies, like topical agents or light treatments, have proven ineffective.
Injectable medications must be prescribed by a healthcare provider and are typically administered in a clinical setting. Due to potential serious side effects, these treatments require careful monitoring by a medical professional. Additionally, be mindful that they can interact with other medications you may be taking.
While there is currently no definitive cure for psoriasis, effective symptom management, reduction of flare-ups, and enhancement of overall quality of life are achievable with the right strategies. Engage with your doctor to create a personalized treatment plan, and don’t hesitate to lean on friends, family, or support groups for assistance. Remember, you are not alone on this journey, and with the appropriate resources, you can regain control over your condition and lead a fulfilling, healthier life.